What is Syndrome Evaluation System?
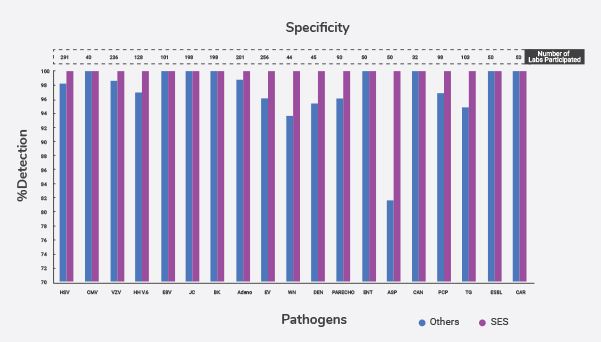
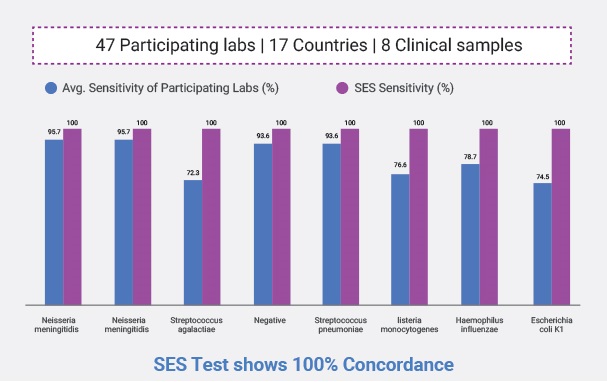
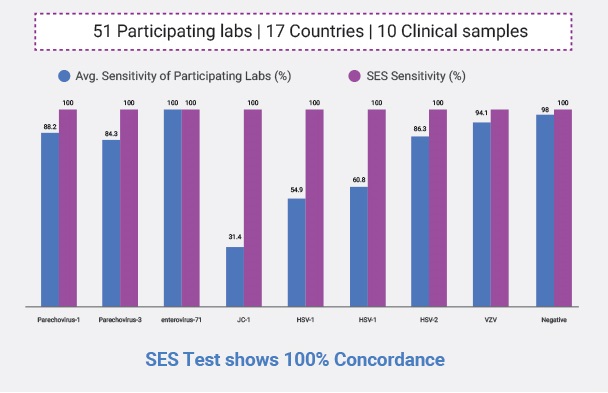
A patented technology that comprises of rapid multiplex amplification and accurate identification of the virulence associated genes of the causative agents or organisms. This amazingly fast and accurate platform transcends all conventional diagnostic tests and helpful when organisms are difficult to cultivate or difficult to find. The technologies currently available for diagnosis of infections are grossly inadequate to detect early during the illness and to institute specific therapy in critical illnesses, resulting in loss of function or even loss of life. The amplification of the gene allows for higher sensitivity of the test and the re-naturation of the amplified signature gene to its chemically identified complementary gene sequence on the SES allows for higher specificity of the test. And the simultaneous detection of multiple pathogens allows for early diagnosis of the infection and initiation of therapy
Prevalence

- According to WHO, 1 in 10 patients get infection while receiving care globally
- The burden of HAI (healthcare associated infection) is several folds higher in low- and middle-income countries than in high-income ones
- Globally, more than 50% of surgical site infections can be antibiotic resistant. In low-and middle-income countries, 11% of patients who undergo surgery are infected in the process
- A systemic infection is being spread throughout the systems of the body as compared to local infections where the pathogen or symptoms are localized in one area. Systemic infections can also be as severe as local infections & life threatening
Common Disorders
Sepsis
- Sepsis or blood poisoning is the leading cause of death in intensive care units. It affects over 26 million people worldwide each year. 258,000 people die from sepsis every year in the U.S. alone. It is the biggest contributor to healthcare associated cost. In India, 1 out of 4 patients admitted in ICU get sepsis, 50% of them die. As many of these patients receive antibiotics prior to getting admitted to the hospitals & ICUs, only in 15% of the patients the causative agents are identified by blood culture. Most of the patients are treated with multiple broad-spectrum antibiotics. 62% of sepsis patients need readmissions. 50% of sepsis survivors suffer from post sepsis syndrome. Early diagnosis and institution of appropriate antibiotics remarkably improves survival rates among patients. SES detects bacteria and fungi four times more than culture within a day while culture takes 3-4 days
Transplant Infections & Febrile Neutropenia
- When patients with blood and other cancers are treated with chemotherapy their white blood cells get drastically reduced making these patients very vulnerable to many serious life-threatening infections. Mortality in Febrile Neutropenia ranges from 11-25%. Early diagnosis is key to successful management and conventional diagnostics detect nearly 17-20% of cases but are not adequately sensitive to rule out the infections to enable clinicians to reduce toxic antibiotics and antifungals (deescalate). In India there is a need for 200,000 kidney transplants, 50,000 liver transplants and 50,000 heart transplants per year. Currently India more than 20,000 transplants annually are carried out. In order to retain the transplanted organ and prevent rejection all these patients are kept on long term immunosuppression. This in turn leads to frequent episodes of life-threatening infections in these patients. Timely diagnosis and appropriate intervention are key to keep these patients safe and functional




 Enquire
Now
Enquire
Now