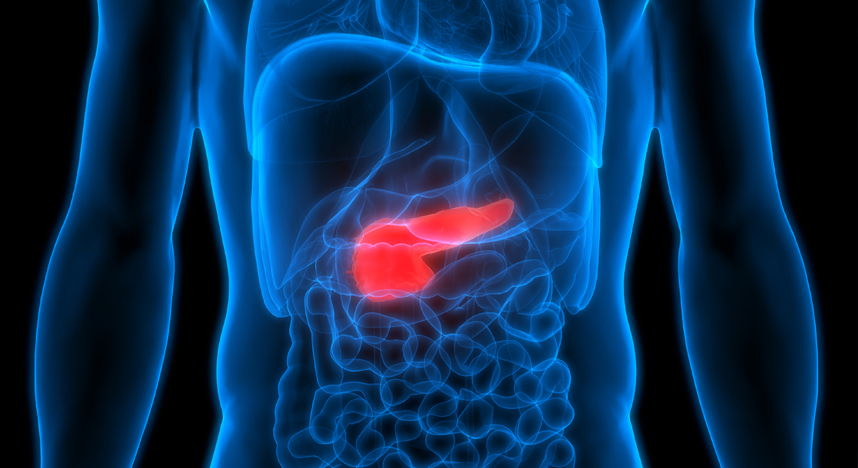
The pancreas is a gland, located behind the stomach, which produces digestive juices and hormones that regulate blood sugar. Pancreatic cancer is the twelfth most common cancer in the world (along with kidney cancer), with 338,000 new cases diagnosed in 2012. The early stages of this cancer do not usually produce symptoms, so the disease is generally advanced when it is diagnosed. The estimated 5-year prevalence of people in the world living with pancreatic cancer is 4.1 per 100,000. This cancer is almost always fatal, and is the seventh most common cause of death from cancer. About 55 per cent of pancreatic cancer cases occurred in more developed countries, with the highest incidence of pancreatic cancer being in Northern America and Europe; and the lowest incidence in Africa and Asia1.
Adenocarcinoma is the most frequent type of pancreatic cancer; slower-growing endocrine tumors account for only a small fraction of the total burden of disease. As for nearly all cancers, incidence rates of pancreatic cancer vary among countries, with approximate 5- to 7-fold differences between countries with the lowest and highest incidence; rates reported from African countries are low because of insufficient data3.
In 2015, it is estimated that there will be 48,960 new cases of pancreatic cancer and an estimated 40,560 people will die of this disease2. The global annual incidence rate for pancreas cancer is about 8/100,000 persons3.
Genetics of Pancreatic Cancer
Pancreatic cancer has been associated with a number of environmental exposures and factors. One such factor is smoking. Established results show that smoking contributes to atleast 20-30% of all pancreatic cancers. Passive smoking also can increase the risk of pancreatic cancer, since environmental tobacco smoke (ETS) contains the same toxins like nicotine, carbon monoxide, ammonia and benzene. Other factors associated with pancreatic cancer are alcohol consumption, diet, obesity, diabetes mellitus, blood type and exposure to certain types of drugs like medication.
A genetic predisposition to the disease is a major risk factor for pancreatic cancer. Activation of the oncogene KRAS, with simultaneous inactivation of the tumor suppressor genes p53, DPC4, p16 and BRCA2 have been associated with the onset of pancreatic cancer. 90% of all cases of pancreatic cancer have p16 mutations, 70% have p53 mutations, and 55% have DPC4 mutations 4.
Around 10% of pancreatic cancers are hereditary, many of which occur as part of rare medical syndromes such as familial breast cancer, Peutz-Jeghers syndrome, familial melanoma, hereditary colon cancer, hereditary pancreatitis, Ataxia telangiectasia and familial pancreatic cancer5.
MedGenome’s Solutions
MedGenome, a provider of clinical genomics solutions for personalized healthcare, offers comprehensive genetic diagnostic solutions for early detection of pancreatic cancer. The solutions provided range from single gene testing to testing a panel of genes (oncogenes and tumor suppressor genes) implicated in the onset of the disease.
Our Hereditary Cancer panel covers all the major genes linked to pancreatic cancer like KRAS, TP53 and STK11. Early detection of cancer is the most important step in ensuring a favorable prognosis, and timely surgical intervention can reduce the risk of developing cancer by up to 85%.
References
- http://www.wcrf.org/int/cancer-facts-figures/data-specific-cancers/pancreatic-cancer-statistics
- http://seer.cancer.gov/statfacts/html/pancreas.html
- Yadav, Dhiraj, and Albert B. Lowenfels. “The epidemiology of pancreatitis and pancreatic cancer.”Gastroenterology6 (2013): 1252-1261.
- http://www.pancreaticcancerindia.com/files/hp/risk_factors.html
- http://pathology.jhu.edu/pc/basicheredity.php?area=ba

 Enquire
Now
Enquire
Now